For postpartum women, there are core dysfunctions that can result in pain, discomfort, pelvic floor symptoms, decreased function and a general frustration. As a note prior to diving in, this is not to be viewed as medical advice and I always recommend consulting with either your medical provider or a pelvic floor physical therapist who can diagnose and treat you accordingly. My advice is general and specific to exercise ONLY.
Between your rectus abdominis is a connective tissue called the linea alba, and this tissue stretches as the two halves of your rectus abdominis separate. As your trimesters progress, DRA becomes more prevalent amongst mamas, and almost 100% have it by the time they give birth.
What Is Diastasis Recti?
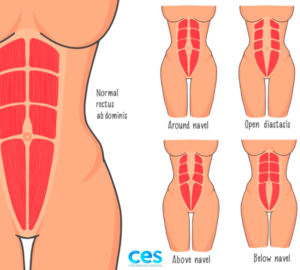
Diastasis recti (DRA) is the separation of the left and right side of the rectus abdominis and the thinning of the linea alba (the connective tissue that meets in the middle from your pubic bone all the way up to your ribs).
Diastasis during pregnancy is a normal adaptation our bodies make to create space for our growing babies. 100% of women will have a diastasis if they make it full term, even after taking preventative steps during pregnancy. It is also a absolutely normal and common part of recovering postpartum.
Some will heal their DRA without any rehab and it may not be present by the 6 week appointment, however, others may need specific exercises to heal theirs. Studies have shown that if a DRA is still persistent after 8 weeks postpartum (which can be anywhere from 50-60% of women) the chance of it spontaneously healing without intentional rehab exercises, becomes much lower.
How do you know when it has healed?
There is a lot of fixation on the gap but the depth (density of the tissue) is just as important, if not more. If you have a separation that is wider than 2 fingers and any softness in the linea alba – more than a knuckle deep- you will likely need specific exercises to help heal your diastasis. If the gap is greater than 2 fingers BUT the density of the tissue increases and can manage intra-abdominal pressure then your DRA can be considered functional. Having a gap DOES NOT mean you core is not functional or ‘broken’. There is so much new -and ongoing – research coming out in regards to DRA and recent studies are now showing that the smaller the gap does not equal higher function.
The depth or squishiness of diastasis is affected by your deep core -transverse abdominals and pelvic floor- and the width is affected by rectus strength. The location of a diastasis and where the separation is can vary per individual (as shown in the diagram above).This is why you need to check width and depth below, at and above the naval.
How do you heal a Diastasis Recti?
There is not a specific list of exercises that will heal your DRA. Any fitness professional claiming an exercise will heal your diastasis, is using it for clickbait. Every postpartum body is different and a one size all approach fits no one well. Instead of having a list of ‘diastasis safe exercises’, focus on movement approaches and strategies you can begin to address and implement into your training.
STEP 1: Connect to your deep core muscles through your breath
You probably have heard that diaphragmatic breathing is your best friend early postpartum. Learning how to breathe with your entire abdomen, side body AND back body is key! However feeling that full expansion in your side and back body can be a struggle for so many women.
Hands and Knees Breathing
A great position to learn how to breathe into your back body, back of your pelvic floor, relax neck and traps and exhale from the bottom up
Side Body Breathing
My favourite position for rib mobility and really feeling your sides expand on the inhale. You should feel a gradually build of pressure on your hands on the inhale, and your ribcage drop on the exhale. Try x10 breaths on each side here.
Deep Squat with Back Body Breathing
Position encourages breath to the back of your body (think breathing into your bra line) as well as the back of your pelvic floor. You can add a yoga block to increase comfort if needed.
STEP 2: Posture/Alignment
Changes to our bodies during pregnancy stem from the growth of the uterus along with physical and hormonal changes that directly affect posture, ligaments and joints. Hormones such as relaxin cause laxity in the joints, particularly the pelvis (to make space for babies exit), which can lead to pelvic and lower back pain during and post pregnancy. As your bump grows, positions of the pelvis and ribcage alters and tilts to allow space for baby and shifting organs. This shift in alignment will leave core muscles stretched, and the laxity means pelvic stability is challenged. Your glutes, hamstrings and back muscles tend to weaken, hip flexors tighten as they work to stabilize, pelvic floor strength and tone diminishes. This ‘mom posture’ doesn’t just disappear overnight once your baby arrives.
During postpartum, you’re also adding hunching over to breast/bottle feet, carrying our increasingly heavy babies on the shoulder, hips, front of body while leaning back, and an overly forward head and neck. During this phase, awareness of your alignment during everyday movements and exercise, along with where you are holding tension, will aid in a faster recovery. Aswell healing a DRA, addressing posture will help strengthen your glutes and back muscles, retrain the pelvic floor and core function and realign your body.
Some things to avoid in your everyday:
- Let go of your glutes. It’s common for women to unintentionally squeeze their glutes when doing things like washing the dishes, or standing holding their baby. If your glutes are clenched, it’s likely your pelvic floor is too.
- Sticking your hips forward to create a perch for your baby. This causes more stress on your already weak midline and can prevent healing. You’re also going to feel your low back working over time. Instead, stand tall with your weight shifted over your entire foot.
- Stop sucking in your abs
- Avoid sticking your rib cage forward, it prevents a good inhale!
- Sometimes you’ll feel better just by switching things up or spending time standing a different way.
- Check-in a few times a day. Small changes over time yield results. Don’t get hyper-vigilant. That just yields anxiety
STEP 3: Connect To Your Deep Core and Pelvic Floor
The exercise selection is second to your breath strategy and your ability to manage pressure and connect to your deep core/pelvic floor.
It also requires you working in a variety of positions & planes of motion. Supine is a great place to start, but you will find you do not progress plateau’s if you’re just doing marches and heel slides for weeks on end.
Don’t fear twisting/rotating, front loaded exercises or lifting weights. Your muscles and connective tissue need to be challenged (appropriately) to heal.
Here are some examples of basic core exercises you can do early on in your recovery as a progression from supine.
STEP 4: Progressive Overload
Just because you may present a diastasis does not mean your core is dysfunctional until the gap has closed. Nor does it limit your strength capacity. Feeling afraid and broken because of diastasis is only natural, but it is not true. If we approach healing a diastasis with fear, then our healing experience becomes stressful, worrisome and disempowering. Yes, rehab work is the approach to start with, but as your body adapts to the stress placed on it, you will need to gradually increase the intensity of your core training. Holding back due to fear will only slow your recovery.
Increase demand by loading movements. An increase in strength = improved density of our muscles, tissue and bones = the ability to manage pressure, withstand more demand and support healing. This applies when you are healing diastasis too. Switch up how you hold the weight (on one side, front rack, goblet hold etc.
Change position: all fours, side-lying, tall or 1/2 kneeling, standing. This changes the gravity demands and will require more stability.
Do more than direct core work! Squats, deadlifts, push, pulls etc all demand you to work your core.
The good news is a diastasis will heal the stronger you get. For some women, this can be weeks and for others it may be months – there really is no time limit to your healing.
If you are struggling to heal a diastasis with these steps, that’s when I would recommend seeking specific guidance from pelvic floor PT and a pre/post natal certified personal trainer.
I’m deeply passionate about helping women feel strong, informed, and confident through every stage of motherhood. You deserve more than just a list of do’s and don’ts or generic modifications. With years of hands-on coaching across all kinds of athletes and clients, I blend real-world experience with specialized pre and postnatal knowledge to create strength programs that go far beyond basic adjustments. This is high-level, accessible training - built for your body, your season, and your goals
EXPLORE MORE POSTS