Prolapse? Or experiencing pelvic floor heaviness early postpartum? It can be challenging to know how to approach your strength training and knowing if what you are doing in the gym is benefitting you, or making your symptoms worse. Before discussing the layers to strength training with prolapse, it’s helpful to understand what prolapse actually is. Let’s dive in…
What is Prolapse?
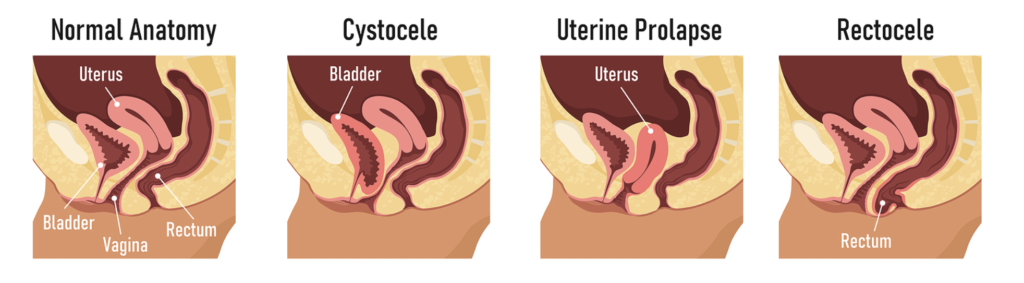
Pelvic organ prolapse, or POP, occurs when pelvic organs such as the bladder, uterus or rectum begin to lose their position in the pelvis and push into the vaginal space. Up to 50 per cent of postpartum women have prolapse. It is a complex diagnosis and there are many factors at play in terms of causes; from structural weakness, damage incurred during labor (ie prolonged pushing, episiotomies, forceps) etc. It’s important to note that POP can happen from issues such as chronic constipation, hysterectomy and advancing age also.
Stages of Prolapse
There are different degrees of prolapse, ranging from minor to severe that can be identified by a pelvic health physical therapist:
- Stage 0 (no prolapse)
- Stage 1
- Stage 2
- Stage 3
- Stage 4 (bulging out of the vagina)
For many women this can feel like a devastating diagnosis. Some women can tell if the slightest thing feels wrong or different with their vagina and seek help. On the flip side, a lot of women have it and never know. They may have never heard of prolapse, or assume that these are all ‘normal’ symptoms from childbirth. It can also be missed by your OB at your 6 week appointment, especially if they are only checking when you are lying down and not when you are standing up and responding to pressure from gravity. During this check, they will not be checking how you tolerate loading your body, whether thats by picking up/carrying your baby/toddler or during exercise. Therefore, because the OBGYN has cleared you early postpartum, many assume all is well even if showing symptoms. If you start noticing symptoms appear, it’s important to get it checked again as prolapse can happen at any time.
Signs and Symptoms:
- Urinary incontinence
- Difficulty with bowel movements
- Painful sex
- Discomfort walking
- A feeling of heaviness, a sensation of something being there, like you’re wearing a tampon or pressure in your pelvic floor
- You can feel or see your pelvic organs bulging out of the vagina.
Types of Prolapse:
The three most common types are:
- Bladder or urethral prolapse: a bulge on the front vaginal wall which can be associated with stress incontinence (leaking with jump/sneeze). It is usually not associated with pain or increased UTI feelings. Pain and UTI type feelings are generally caused by muscular tightness in the front of the pelvic floor and not the prolapse itself. Once the tightness decreases from relaxation and lengthening techniques, the symptoms usually go away, even if the prolapse remains unchanged.
- Stage 1: the bladder protrudes a little way into the vagina;
- Stage 2: the bladder protrudes so far into the vagina that it’s close to the vaginal opening;
- Stage 3: the bladder protrudes out of the vagina;
- Stage 4: the pelvic organs, including the bladder, protrude out of the vagina.
- Uterine prolapse: occurs when pelvic floor muscles and ligaments stretch and weaken and no longer provide enough support for the uterus. This can cause some low back pain and you may feel a “heavy” sensation.
- Stage 1: the cervix drops into the vagina;
- Stage 2: drops to just inside the opening of the vagina;
- Stage 3: the cervix is outside the vagina;
- Stage 4: the entire uterus is outside the vagina.
- Rectoceles: a posterior vaginal prolapse that occurs when the supportive wall of tissue between a woman’s rectum and vaginal wall weakens and the front wall of the rectum bulges into the vagina. Note – this is different to rectal prolapse, where the rectum protrudes through the anal opening. Often, woman have no symptoms, however it can also feel difficult to have a bowel movement, you may experience rectal fullness or pressure, and like something is falling out of your vagina.
All types of prolapse can cause a sensation of something being “there,” and mentally that feeling is very bothersome.
Strength Training and Prolapse
Early Postpartum:
Learn how to breathe. Optimal diaphragm function is the foundation for optimal core and pelvic floor function.
Assess your pelvic floor: find a local pelvic floor physical therapist who assess whether your pelvic floor muscles are tight, weak, strong etc. You may need some release work, you may need some strength, you may need both.
Learn how to manage pressure: understand what it feels like to ‘bear down’ and whether you are doing it during exercise, during bowel movements or with everyday activities. This is SO important for your recovery.
Elevate your hips: counter gravity but elevated your hips and taking pressure off your pelvic floor. So much of that initial postpartum recovery is heavy on mind-muscle connection and often it can be difficult for women to feel themselves let go. This can also be a relief if you notice pelvic floor tension after being on your feet a lot.
Start with basic breath work and then progress movements. Here are some ideas of how you can include some early core and pelvic floor rehab with your hips elevated:
Considerations for Strength Training:
-Prolapse does not mean you should not strength train. In fact, it’s a great opportunity to get stronger. We need this strength to lift and carry our baby/toddler.
-Focus on building hip, glute, adductor and core strength. These muscles work WITH your pelvic floor and help ensure optimal function.
-Eliminate any exercises in your workout(s) that cause too much pressure on your pelvic floor. There is no magical position that works for everyone, or position/exercise that is unsafe as it will vary for everyone. It’s how YOU can manage or tolerate the movement.
-It is important to be able to move through exercises that mimic daily life while controlling pressure. For example, squatting and deadlift happen so many times throughout the day and if you are bearing down to lift you baby/toddler every time, you may find symptoms aren’t improving. Start simple, begin movements without any load, limit range of motion and difficultly by adding a box to the bottom of lower body exercises, switch up how you are loading the exercise, exhale through full range of motion or on exertion.
HOW TO MODIFY SQUATS/DEADLIFTS: Remember, these are GUIDELINES and may not work for you.
- Squat to Box
2. Suitcase Squat/Deadlift to Box. You can also do this with a typical deadlift load in front of you too if helpful.
3. TRX Squat/Single Leg Squat to Box: similar kind of method, except using some upper body support to help you too.
BUILDING STRENGTH: Adductors
Our adductors (inner thigh muscles) are one of the many components that aid in pelvic floor function as well as contribute to pelvic floor issues. They can either help our pelvic floor out or make it do more work. It is important to keep these muscles flexible and strong during pregnancy and into postpartum, versus tight and weak. It’s likely that with a pelvic floor dysfunction you have one adductor stronger than the other.
Therefore, squeezing a ball between your thighs a great tool to help you engage your inner thighs. Here are some exercises that intentionally activate the pelvic floor, inner thigh and core. I’ve chosen movements that are side lying and single leg/side focused to feel the difference in strength/weakness/tightness from side to side.
Side Lying Adductor Squeeze: Start in side lying position. One hand supporting your head, other on rib cage. Work on feeling that side body expansion as you inhale. You should feel your breath push against your fingers. As you exhale, lift pelvic floor and push your top leg down onto the ball. You should feel your inner thigh and deep core activate.
Dynamic Copenhagen Side Plank: set up with your head perpendicular to a bench and facing away. Plant your elbow and forearm parallel to the bench, placing your front leg (bent) on top. As you exhale, lift up your hips so you’re in a straight line from the ankles to the shoulders. As you do this, also lift your bottom leg up so it’s parallel to the ground. Keep this movement dynamic, pushing with your top leg on the bench to lift and lower.
Glute Strength:
1/2 Kneeling Cable/Banded Rotation: Set up in a 1/2 kneeling position, cable at chest height. On your inhale, open towards the anchor point feeling your hips open and upper back move. On the exhale rotate towards your front leg. Arms should slightly cross your front leg.
Lunge Rotation: Once you have mastered this movement in a tall kneeling or 1/2 kneeling position, as well as your Pallof press, you can progress to making it more dynamic. Start in a lunge position, outside leg forward. As you exhale, lower into your split squat, bring your arms down and across your front knee. Keep rib cage stacked over pelvis and front leg stable/in place without the knee collapsing in. As you stand, return your arms towards the anchor point. Your upper body and hips should rotate. This is a great movement for hip internal rotation, adductor, core & pelvic floor strength.
Single Leg Glute Bridge (Feet Elevated): Elevating your will remove gravity from the exercise and may make this easier. You can also choose to do this with your feet on a wall or the floor. Start by lying on your back knees bent. Rib cage and pelvis are aligned throughout the movement. As you exhale to extend your hips, core engaged. Inhale as you lower your hips and return to your starting position.
All of the exercises shown are examples of how to strengthen those particular muscle groups or modify movement patterns. They are not necessarily ‘prolapse safe’ or a hard list to follow. As mentioned, prolapse is a complex diagnosis that goes way beyond exercise selection so make sure you speak with either your provide or a pelvic floor physical therapist. You can find one local to you HERE
I’m deeply passionate about helping women feel strong, informed, and confident through every stage of motherhood. You deserve more than just a list of do’s and don’ts or generic modifications. With years of hands-on coaching across all kinds of athletes and clients, I blend real-world experience with specialized pre and postnatal knowledge to create strength programs that go far beyond basic adjustments. This is high-level, accessible training - built for your body, your season, and your goals
EXPLORE MORE POSTS